
At Home Remedies for Dry Mouth
When the mouth isn’t producing enough saliva, it can make things uncomfortable. Dry mouth makes you feel like your tongue is sticking to everything it touches, you can’t talk or eat normally, and your lips can be chapped and begin to crack. Not to mention, it can also cause bad breath. Sometimes, it can be caused just by everyday stress and anxiety, however sometimes it’s your body’s way of telling you something deeper is wrong. Keep reading to learn more about dry mouth, and how you can try to treat it at home!
What is Dry Mouth?
Xerostomia, also known as dry mouth, can drive you crazy if left untreated. If you’re not making enough saliva, your mouth will feel perpetually dry. Fortunately, there are many at home tips to prevent this from happening like staying hydrated, trying mouthwash, and other over the counter products.
What Does Dry Mouth Feel Like?
When salvia production is decreased the mouth becomes sticky. It can be mild or severe, but it can cause complications if not taken care of. If you think you are suffering from this, see if you have any of these common symptoms:
- Dryness that often makes the mouth feel sticky
- Thick saliva
- Bad breath
- Inability to chew, speak, or swallow easily
- Sore throat or hoarseness
- Dry tongue
- Altered sense of taste
- Problems with dentures
What Causes This?
A dry mouth can be the result of a number of different things. Healthline details the most common causes of this to be:
- Dehydration can cause this because there’s not enough fluid in your body to develop salvia properly
- Stress and anxiety make the body more prone to acid reflux and similar symptoms, leading to having this feeling
- Smoking and using tobacco products and things of the like can increase dryness
- Taking antidepressants, antihistamines, or diuretics affects how the saliva is produced, but in most cases it will return to normal when medication is stopped
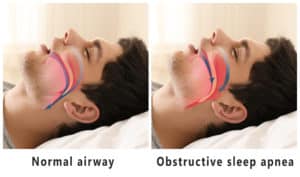
- Breathing through your mouth like when snoring can remove moisture from the mouth
- Radiation or chemotherapy can sometimes change the amount of saliva produced. Radiation can also damage the salivary glands when used on your head and/or neck. Depending on the dosages, this could be temporary or a permanent side effect
- Autoimmune disorders like Sjogren’s Syndrome can affect the glands that make saliva
- Food poisoning can cause dehydration, which in turn causes a moisture-less mouth
- As we grow older, our body changes how it processes medications and more. This can mean being more susceptible to experiencing this side effect
At Home Remedies
When your mouth is dry, you can try some at home remedies to see if that helps relieve the irritation. Mayo Clinic provides the top remedies to help your dry mouth:
- Try chewing sugar-free gum to stimulate the flow of saliva
- Limit caffeine because caffeine has been linked to causing dry mouth
- Don’t use alcohol-based mouthwashes which are notorious for drying out the mouth
- Quit smoking and chewing tobacco
- Drink water regularly throughout the day to keep hydrated
- Use over-the-counter saliva substitutes such as mouth moisturizing sprays to help boost the moisture in your mouth
- Use a mouthwash specifically made for dry mouth
- Be weary that over-the-counter antihistamines and decongestants can elevate dry mouth symptoms
- Trying to breath through the nose and not your mouth
- Bring a humidifier into your room while you sleep
If you have a dry mouth, it could be the side effect of a deeper problem. This is why it’s important to check in with your dentist so you can get to the bottom of cause. Other tips to remedy this at home include limiting sugary and acidic food and beverages, use fluoride toothpaste and rinses, and make an appointment to see the dentist at least twice a year.
Dry Mouth Complications
If left untreated, this can sometimes cause further complications which can be severe. Complications include increased plaque, tooth decay, mouth sores, yeast infection in your mouth, sores, cracked lips, and poor nutrition from not being able to intake adequate nutrition through eating.
Make an Appointment
Your oral health is important. If you are suffering from a dry mouth and can’t find adequate relief through these at home remedies, request an appointment today. Dr. Ania and her team will look for the underlying cause to develop the best treatment plan for you and your symptoms. During your exam, Dr. Ania will go over all your symptoms with you so she can get you better quickly. To schedule your exam for dry mouth, call Dr. Ania’s office at (303)-872-9940.



























 Signs and Causes of TMJ Disorder
Signs and Causes of TMJ Disorder
 Help for Your Symptoms
Help for Your Symptoms